ABOUT
Nerve Conduction Studies
The NCS is a test that elicits a response from the nerve cells and muscles in the extremities. It measures the response in velocities, amplitudes and latencies. The diagnostic focus is on radiculopathies, neuropathies, demyelination of the nerve and axonal loss. The motor and sensory components of the nerve are evaluated. From this data we can identify the approximate location of the nerve injury or lesion.
The Nerve Conduction Study consists of:
- Nerve Conduction Velocities (NCV), F-Wave and H-Reflex
- Dermatomal Somatosensory Evoked Potentials (DSEP)
- Electromyography (EMG)
Integrity of the nerve is diagnosed by the following criteria:
- Reaction time (latencies)
- Velocities of the effected nerve
- Amplitude of the captured waves
- Muscle innervation by the nerve

- Objective and reproducible findings that can pinpoint the lesion to the nerve
- Provides an excellent differential diagnosis
- Can help further diagnose disease
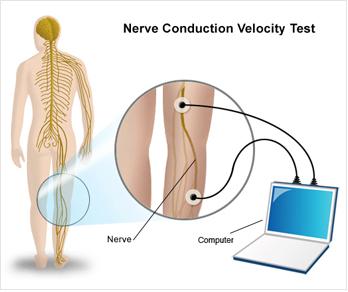
Nerve Conduction Velocity (NCV) is used to measure action potentials resulting from peripheral nerve stimulation. The reaction times (latencies) and velocities obtained will detect neurological problems or compression of the nerves throughout the extremity.
The F-Wave looks at the most proximal segment of the nerve, including the root. The reaction time (latency) will show if there is a delay at the spinal level of the particular nerve.
The Tibial H-Reflex is considered to reflect that state of the S1 nerve root and its sensory component.
Collectively, the F-Wave and H-Reflex look at compression at the cord level.
By testing both the motor and sensory components of the nerve, a doctor can obtain a comprehensive picture of the patient’s problem areas.
“The clinical utility of Nerve Conduction Velocities (NCV) is based upon its ability to: 1) demonstrate abnormal sensory function when the history and/or neurological examination are equivocal; 2) reveal the presence of clinically unsuspected malfunction in a sensory system, when demyelinating disease is suspected because of symptoms and/or signs in another area of the Central nervous System (CNS); 3) help define the anatomic distribution of a disease process; and 4) monitor objective changes in a patient’s status.
These tests provide reproducible, sensitive, quantitative extensions of the clinical neurological examination…NCV’s are essential to the modern practice of medicine because they: 1) provide data unobtainable without the use of amplifiers and oscilloscopes; 2) quantify and objectify data which the clinician may sense; 3) localize lesions within a long sensory pathway; 4) are more efficient and cost-effective because the testing is done by paramedical personnel who can be trained more expeditiously than neurologists, ophthalmologists and otolaryngologists.”
- Chiappa, M.D., Evoked Potential in Clinical Medicine, (condensed and reprinted).
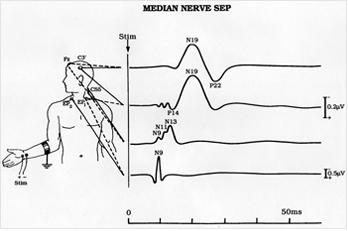
Dermatomal Somatosensory Evoked Potential (DSEP) involves mild stimulation of the sensory nerves in a dermatomal region and records the reaction time to the cortex. DSEP looks for nerve root compression.
“For most neurological problems, two issues addressed by somatosensory evoked potentials (SEPs) are the verification of a conduction abnormality and the localization of that abnormality along the neuroaxis. Conventional SEPs to mixed nerves stimulation may adequately verify a conduction abnormality, but not its location. From a technical standpoint, DSEPs are easier to record than Spinal SEPs and could serve as a useful technique for localization of neurological abnormalities along the neuroaxis.”
Jefferson C. Slimp, PhD, et al, “Dermatomal somatosensory evoked potentials: Cervical, thoracic and lumbosacral levels.” Electroencephalography and Clinical Neurophysiology.
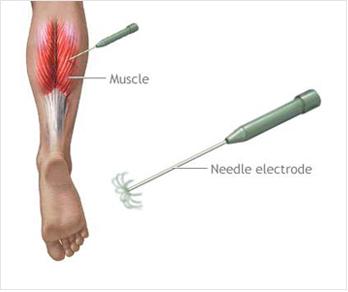
Needle Electromyography (EMG) is offered in conjunction with the nerve study.
Electromyography tests the integrity of the entire motor system, which consists of upper and lower motor neurons, the neuromuscular junction and muscle. It is an invasive technique that requires needle insertion and adjustment at multiple sites. Activation of the motor unit will cause a potential wave form from the recording needle, as well as audible sound, which is also diagnostic. Depending on our findings, at least five muscles will be tested that correlate with the specific nerve distribution of the affected area.
Electromyography (EMG) studies the intrinsic electrical properties of skeletal muscles.
- Carpal Tunnel Syndrome
- Cord Trauma
- Disc Disease
- Hyperflexion/Extension Injury
- Nerve Entrapment/Neuropathy
- Nerve Root Irritation
- Neuritis/Sensory Deficits
- Peripheral Nerve Trauma
- Plexus Stretch Injury
- Radiculitis
- Sensory Dysfunction
- Sciatica/Radicular Pain
- Spinal Stenosis
- Systemic Neuropathies
- Tarsal Tunnel Syndrome
- Thoracic Outlet Syndrome
- Vertebral Subluxation Complex
